Anyone familiar with Pope Paul VI’s Humanae Vitae or Theology of the body should know about natural family planning. It’s a natural, non-invasive, and healthy means of achieving or avoiding pregnancy. It is NOT the rhythm method! Here’s the overview from our latest book: Paleo Family: Raising Natural Kids in an Unnatural World.
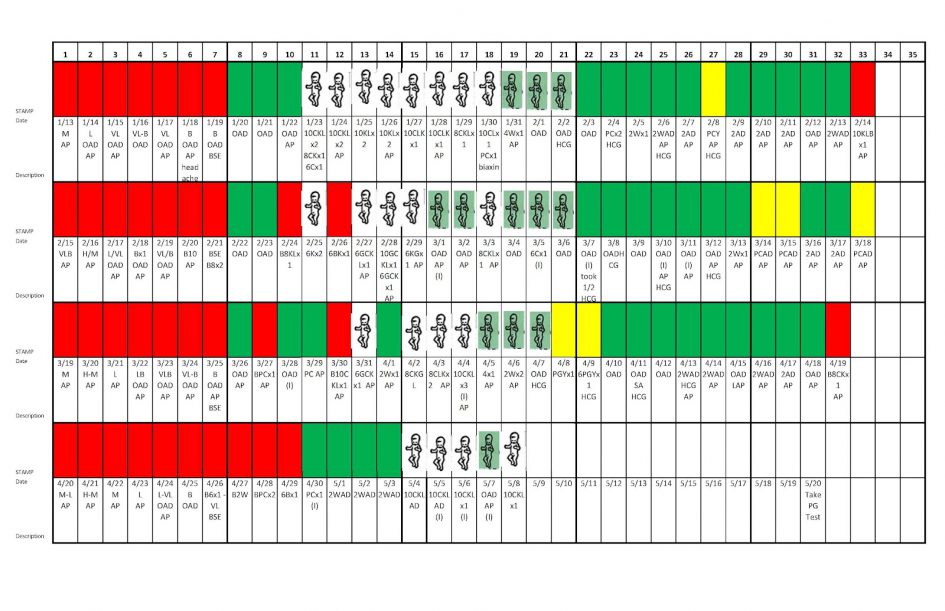
The couple’s coach looked up from the chart and, with a smile, congratulated them on their first child. They looked at each other quizzically, but the coach repeated her congratulations. Mom was just a few days pregnant and her coach was the first person on Earth to know—preempting even mom—and she knew it simply by looking at a piece of paper that contained a row of colored stickers marked with cryptic messages. The first few stickers were red, followed by several green stickers and then some clear.
This wasn’t Miss Cleo reading their fortune off some Tarot card, this was real biological science and it worked. The coach was a clinician specially trained in Creighton Model fertility monitoring and Natural Procreative (NaPro) Technology, a natural and inexpensive method of tracking fertility and treating conditions that inhibit conception. And while that couple in particular was using the techniques to achieve conception, it’s just as effective at preventing pregnancy.
Perhaps you are not ready to grow your Paleo Family just yet, but want a non-pharmaceutical, non-surgical method to temporarily avoid pregnancy that is just as effective. In healthy women, there is usually only a short period of about a week when she is capable of conceiving. This window is recognized by several physiological indicators that can be identified through simple observation and one that requires more substantial testing. In most cases, before ovulation, a woman’s basal temperature drops predictably and she produces a specific type of vaginal discharge known as fertile-type mucus. Both of these changes can be monitored for very little or no cost. These changes are brought about by a change in the bodily endogenous hormones estrogen and progesterone, which can be further measured through blood samples in atypical cases.
Women can track these physiological processes on a mobile app or, as the couple mentioned above did, on paper using a color-coded sticker system. The result is a series of stickered rows with notes on the fertile days indicating what type of fertile mucus is present. A certain quality of fertile mucus indicates ovulation is forthcoming. The obvious takeaway is that if a woman is trying to avoid pregnancy, she should abstain from sexual intercourse during her fertile (clear) days, especially the peak fertility days. If she is trying to achieve pregnancy, she should have sexual intercourse on her fertile days and especially peak fertility days.
If you’re interested in natural fertility monitoring, it is recommended to find a method backed by scientific research and locate a trained professional in that method for education and consultation, many of which are offered online. The four most popular and successful methods with available resources such as classes, websites, and personal coaches/practitioners include: Symptothermal, Billings Ovulation Method, Creighton Model Fertility Care, and Marquette Model. Symptothermal method uses basal body temperature, cervical mucus observations, and cervical position to indicate days on which a woman is fertile. Both Billings and Creighton rely on observations of cervical mucus and vaginal sensation; but Creighton requires more detailed observations and is the only method that can be used in conjunction with NaProTechnology to diagnose and treat hormonal and gynecological conditions such as polycystic ovarian syndrome and endometriosis. Marquette requires the purchase of a fertility monitor, which is highly effective when used in conjunction with observation of mucus and basal body temperature.
The success rate of these methods when used correctly to avoid pregnancy is often on par with the pill according to research studies. Additionally, the success rate of fertility awareness methods to achieve pregnancy is quite high as well. As we saw in the previous section, hormonal contraception causes weight gain, mood swings, tumors, and a whole host of medical conditions (not to mention ecological and societal effects), yet it’s touted as health care. Knowledge of her personal fertility cycle can not only help a woman discover ways to naturally optimize her reproductive health, but also empower her with knowledge that can lead to a more healthy, drug-free lifestyle.
Paleo Conception
When a couple is trying to conceive but having trouble, it can be stressful and even painful as it was for us. We can only imagine the anguish parents must feel when they can’t conceive month after month, then year after year. Infertility describes a period of non-pregnancy of over 12 months in couples who are actively pursuing conception by having regular, unprotected sex. The World Health Organization’s Scientific Group on the Epidemiology of Infertility has defined infertility as a disease. Typically, infertility is broken down into two categories, primary infertility, which refers to those who are unable to conceive “so far”, and secondary infertility or subfertility, which refers to those that have been previously considered fertile. It’s important to note that infertility or subfertility is different from sterility, which is characterized by the impossibility of conception. But does a classification as infertile mean that a couple will never conceive? Not necessarily. Many can and do go on to become pregnant. Of the 10-15 percent of couples diagnosed as infertile, roughly half go on to conceive within two years of their diagnosis.
In countries like the United States, the most common factor in infertility cases is the increasing tendency of women to wait longer before having children. Of course, it is widely known that women’s fertility does decline with age. In fact, many agree that peak fertility is around 25 years of age in women and starts declining more rapidly after 30 years. Still, evidence suggests that women can (and many do) wait until their early thirties to start trying to conceive. And because there is a general ignorance of fertility awareness methods of family planning and fertility treatments that work with a woman’s natural cycle (Napro Technology is phenomenal), many people turn to methods of assisted reproductive technology like in vitro fertilization (IVF) that are meant to increase the likelihood of achieving conception by a spectrum of unnatural means.
Since its introduction in 1978, over 5 million children have been conceived through IVF, making the program a major landmark in infertility treatment. That equates to about 2-3 percent of births per year. IVF was initially developed in order to make it possible for women with severe tubal blockages to become pregnant. The process involves injections of hormones which stimulate the production of follicles in the ovaries. Then, eggs are collected and placed together in a petri dish with sperm so that fertilization may occur in vitro.
Because of the overall success rates of IVF programs, as well as our society’s growing confidence in artificial fertility technologies, the use of IVF has expanded from its initial purpose as a method of conception for women with tubal blockages to include a number of other factors contributing to infertility, such as endometriosis, male subfertility or infertility, and unexplained infertility in couples. This is significant because 20-30 percent of couples who are classified as infertile are diagnosed without clear explanation and these couples make up a growing number of IVF cases. Recent studies also express major concerns about the economical as well as ethical aspects of IVF. Despite the increase in programs and the number of IVF births, nearly forty years on, IVF—as well as other assisted reproductive technologies (ARTs)—remains unavailable or unaffordable to a large majority of couples struggling to conceive.
A surveillance study by the Center for Disease Control and Prevention (CDC) estimates that the average cost of births as a result of assisted reproductive technologies like IVF amounts to about $27,000 without insurance. Despite these vast sums, research suggests that IVF is currently being overused in couples who might still conceive without its assistance.
Contributing to the concern of the IVF overuse is the suggestion that the procedure might be linked to certain adverse health effects in offspring. Both IVF and intracytoplasmic sperm injection (ICSI) have recently been associated with birth defects, including congenital disease, impaired development, and the risk of retinoblastoma, a rare form of eye cancer found in some children.
Given the cost and potential risk, why does the use of IVF persistently increase? Of course, better access to IVF in recent years, a lack of confidence experienced in patients and couples, as well as a greater trust in technology contributes to the popularity of IVF in the treatment of subfertility. And yet, in couples experiencing unexplained subfertility who begin IVF programs, up to 30 percent will go on to conceive before undergoing any treatment, pointing to society’s overuse of the method. For some couples, there are simple ways of achieving conception without resorting to assisted reproductive technology.
There are a wide number of factors contributing to infertility in women, such as endometriosis and pelvic adhesions. Certain hormonal fluctuations can also interfere with the functionality of the menstrual cycle. The cause of infertility is often (although not always) multifaceted and it is therefore vital that couples do not take on an individual burden of blame for what is typically a shared problem.
One of the most common factors contributing to subfertility is simply a lack of understanding regarding the complexities of conception. In some cases, couples experience infertility as a result of a shortage of knowledge regarding a woman’s “fertility window” and general ignorance of natural fertility science as described previously.
So, what do couples need to understand in order to increase their probability of conceiving without the use of ARTs? Firstly, there are certain “necessities”, including the functionality of a woman’s hypothalamus, which is responsible for the release of certain hormones in the brain, the pituitary, ovarian and thyroid hormones, and the uterus. It is also necessary for men to produce a good supply of healthy sperm, often ranging in the hundreds of millions.
An adequate amount of cervical mucus, which assists the transfer of sperm from the vagina, is also necessary. Mucus production can be interrupted by surgeries, birth defects, or infections. In fact, certain conditions (such as chronic cervicitis, severe inflammation, and congenital disease) can alter the receptivity of cervical mucus. Medications, as well as lifestyle choices (like smoking), can also play a role.
Vaginal pH
Hormonal fluctuations, too, affect the production of cervical mucus and can actually alter the structure of the mucus itself, which then goes on to influence sperm penetrability. A hostile cervical mucus, or an inadequate supply of cervical mucus, can obstruct the passage of sperm.
There are a lot of complex factors to consider here, but there are certain things that women can do to ensure they understand what is going on in their bodies (and in their partners’ bodies). For example, the significant role of vaginal pH (a measurement of acidity or alkalinity) and cervical mucus in relation to sperm function is highly underestimated.
The acidity (or pH levels) in the vagina fluctuate during the menstrual cycle, reaching their most acidic levels around mid-cycle, creating an acidic environment toxic to sperm. That means that sexual intercourse during this period is unlikely to lead to conception. Stress, immunological effects, hormonal disorders or fluctuations (especially in estrogen levels), as well as the use of antibiotics can negatively impact vaginal pH levels in women.
Only about 200 out of 280 million sperm reach the cervical canal following ejaculation. If semen is unable to withstand the acidity of the vagina it can lead to infertility. All of this means that timing really is everything. Under normal conditions the lifespan of an egg ranges between 12-24 hours, while the ability of sperm to survive within the reproductive tract is typically between 48-72 hours and sometimes up to five days. Therefore, pregnancy might not occur if a couple does not time their sexual encounters appropriately.
Fertile Mucus
A thorough understanding of the menstrual cycle is also essential to successful conception, with chances enhanced when a couple has sex just before ovulation. During this period the cervix undergoes a change in size and texture. Due to increased estrogen levels before ovulation the cervix “swells and softens”, externally dilating. It then begins to secrete a larger amount of mucus which is “slippery”, “clear”, and “stretchy”, assisting the sperm to enter the uterine cavity. For those that are not producing enough cervical mucus, doctors can sometimes recommend a small dose of conjugated estrogens in the period leading up to ovulation. There’s also evidence that vitamin B6 supplements can increase fertile mucus. After ovulation, hormones like progesterone cause the cervix to harden, creating a thicker mucus that works to “plug” the uterus and prevent fertilization.
With all that in mind, how can a couple determine the optimal time for sexual intercourse in order to conceive? There are several over-the-counter options which help to predict ovulation. Most pharmacies carry basal body thermometers which, after about three months of careful charting, can help determine when a woman is ovulating. These thermometers work because the release of progesterone during the menstrual cycle causes a slight increase in basal body temperature. During the stage preceding ovulation, basal body temperatures are slightly lower (around 97.2-97.6 degrees Fahrenheit), whereas after ovulation basal body temperatures are around 98 degrees.
Ovulation predictor kits are also widely available and are designed to detect the hormone in the urine that induces ovulation, luteinizing hormone. Some women might need to have certain hormone levels measured if they do not appear to be ovulating regularly. In some cases, there are certain medications which might be taken in order to induce ovulation. Clomiphene citrate (CC) is a cost effective treatment that helps to stimulate ovulation in women with polycystic ovary syndrome. Following the use of CC, about 60-85 percent of women with this syndrome will begin ovulating.
Of course, these tools are able to identify when ovulation occurs but also if there is a hormonal imbalance. Imbalances can be treated with synthetic or bioidentical progesterone supplements which help the body get back to the normal cycle and ovulation schedule.
Hormones aren’t important to just women, though. Abnormalities in male hormone levels can affect his reproduction contribution by decreasing sperm counts and libido. It is necessary for men to produce a certain number and quality of sperm which are also capable of jumping through the hoops—both literal and figurative—of a female reproductive tract. Inadequate supplies of sperm can lead to subfertility.
Infertility in men tends to be the result of four possible factors: genetics, lifestyle, environment, and certain urethro-genital or endocrine diseases. Substance abuse, as well as the use of certain medications (such as chemotherapeutic agents and beta-blockers) can negatively affect reproduction. Even the amount of sex a man engages in can influence the production and quality of sperm, with frequent sex decreasing sperm counts and less frequent sex producing “sluggish” sperm. There is evidence suggesting that vaginal lubricants can negatively impact sperm and should be avoided in some cases of subfertility, though there are lubricants (e.g. Preseed) which are designed to emulate fertile-type mucus and increase chances of conception.
Diet
Diet can also influence fertility during the preconception period. Although infertility is typically the result of a number of factors, research into fertility in countries where women might have nutrient deficient diets demonstrates that there is a correlation between nutrition and fertility rates. These deficiencies can also have a lasting impact on the overall health and well-being of your baby.
Studies show that there is a link between micronutrient supplementation and female fertility. In particular, higher levels of vitamin B6 have been observed in women considered fertile when compared to women experiencing some form of subfertility. Whole grains, vegetables, and animal products tend to be rich in vitamin B6.
Of course, it is not just up to women to maintain a healthy diet during the preconception period. Studies also demonstrate that the nutritional habits of men are linked to fertility rates. Poor nutrition, as well as drug or alcohol abuse, can contribute to subfertility in men. Like nutritional supplementation in women, there are certain things that men can do to both improve their diet and help nurture their fertility.
Men who consume greater amounts of omega-3 fatty acids have been shown to be more fertile than men who consume fewer omega-3s. The consumption of alpha-linolenic acid (found in chia, kiwi seeds, flax or linseed, rapeseed, and soy) can boost sperm count and motility, while the docosahexaenoic acid (DHA) found in omega-3s improves the fluidity of sperm.
Antioxidant support can also boost fertility. Especially when taken with the right concentration of fish oil, antioxidant treatment can positively influence the production of sperm. Other supplements, like zinc and folic acid, have been shown to increase sperm concentration, while vitamin C (especially in smokers) is said to improve the quality of semen. Evidence suggests that the controlled supplementation of carnitine, zinc, folic acid, tocopherol, and astaxanthin can increase fertility rates among men. Women, too, should consider folic acid supplementation as it can decrease the risk for neural tube defects.
While exercising and dieting are generally thought to improve fertility rates among men and women, anything done in excess can have negative implications on fertility. Over-exercising or dieting can cause menstrual disorders and anovulation. The consumption of drugs, alcohol, tobacco, and caffeine can also contribute to infertility. A well-balanced diet and healthy lifestyle is probably the most useful method of promoting general health and, as a bonus, fertility.
Stress may also hinder the chance of conception (although it is rarely the only factor in subfertility cases). In a study conducted by Domar et al, a combination of relaxation techniques, stress management, nutrition, and diet planning, as well as cognitive restructuring, saw nearly one third of women conceive within six months. These women also necessarily reported feeling less anxiety and depression. Even more significant, similar results were recorded when the study was conducted with 50 women experiencing subfertility.
If you have tried these natural treatments at home, please know that artificial reproductive technology is not your only option. There is a natural, medically-researched, and successful way to achieve pregnancy for a plethora of conditions without going the artificial route. It is called NaPro Technology. NaPro Technology (NaPro) is a relatively new women’s health science that aids in monitoring and maintaining a woman’s reproductive and gynecological health by charting any of several of physical and instrumental observations. It views infertility as a symptom, rather than a disease. It requires training in Creighton Model of fertility awareness (mucus only method). Using Creighton Model biomarkers, women can track their fertility with a precision previously thought impossible without expensive medical equipment. As the NaPro website states:
NaProTECHNOLOGY uses the Creighton Model FertilityCare™ System biomarkers to monitor easily and objectively the occurrence of various hormonal events during the menstrual cycle. NaPro tracking provides valid information that can be interpreted by a woman and by physicians who are specifically trained in this system.
Unlike common suppressive or destructive approaches, NaProTECHNOLOGY works cooperatively with the procreative and gynecologic systems. When these systems function abnormally, NaProTECHNOLOGY identifies the problems and cooperates with the menstrual and fertility cycles that correct the condition, maintain the human ecology, and sustain the procreative potential.
With these data, physicians have a better understanding of the root problems of any given subfertility and can address them more effectively through complementary hormone therapy or a specialized surgical procedure like “near-contact” laparoscopy, endometriosis excision, or wedge resection for polycystic ovaries. The heartbreak of infertility is not to be taken lightly and the suggestion that natural methods of treatment is in no way meant to belittle the efforts of those who have experienced years, perhaps decades, of trying to conceive. We sincerely hope that the options described above will help you to find ways to start or grow your little tribe in the healthiest manner possible.
More in Paleo Family:
 The Libertarian Catholic
The Libertarian Catholic